Our individual environmental history – where we live, work and visit – can be linked to our health. Katrina Megget looks at how geomedicine could change the way we diagnose and treat disease
In 1854, an outbreak of the bacterial infection cholera struck the Soho district of London, killing 127 residents in three days and prompting a mass exodus of nearly three quarters of the local population. The cause and source of the outbreak – which many at the time thought was an airborne disease – was unknown. But anaesthesiologist John Snow had a theory. Using a hand-drawn map of the locations of cholera deaths, superimposed with the locations of public water supplies, and alongside information of where the victims sourced their water, Snow pinpointed the Broad Street water pump as the likely source of the outbreak. The pump handle was removed and modern epidemiology was born.
By mapping the outbreak in this way, Snow applied a basic geographic information system (GIS) to relate the disease to a particular location. It’s a method that has been used since, and the beauty of it is the ability to link non-spatial data, such as medical record information or pollutant measurements, to the same location, thereby providing a new layer of insights within the context of geography. From a public health perspective, the implications are vast – finding correlations between health conditions and the geographical areas where people live. And these possibilities are spawning new thoughts on how we approach health.
One person spearheading a new approach using geographic information is Bill Davenhall, a former health and human services lead at California-based GIS specialists Esri, who advocates a new discipline he has coined ‘geomedicine’. This is essentially the capture of information about the environment in which an individual person lives, works and plays, which is then linked to their medical information. With this approach, doctors can tap into a database and determine the patient’s proximity to, for example, known health risks, harmful chemicals, other environmental factors or even socio-economic conditions that could affect health. Davenhall believes a geomedicine approach can build a more accurate picture of a person’s current and future health, thereby improving disease diagnosis and treatment.
A place in history
Every place has its own environmental history, Davenhall explains, and each environment can affect a person’s current and future health. For example, clear evidence shows air pollution is linked to heart disease and asthma, while many studies suggest the number of fast food outlets in a person’s neighbourhood is associated with an increased risk of type 2 diabetes and obesity. A recent World Health Organization report concluded that ‘unhealthy environments are a factor in millions of deaths worldwide’, with deaths from cancer, heart and respiratory disease, diarrheal disease and certain neonatal conditions linked to ‘place’.
[[People move about with little thought about the environment around them]]‘People move about with little thought about the environment around them, especially if it’s not in their face,’ Davenhall says. ‘They seldom know what’s in the ground around them, in the water that comes out of their kitchen faucet or in the air they breathe. The not-so-obvious hazards are often well camouflaged but that does not mean their geographic location is unknown.’ And when conservative estimates claim that 30% of health issues are related to the environment, it’s easy to see why geomedicine is gaining a following.
Ethan Berke at the Dartmouth Institute for Health Policy and Clinical Practice in the US is another supporter of geomedicine, and says it is critical to start considering the context of where a person lives in relation to their health. With an increasing emphasis on healthy lifestyles and disease prevention, Berke says it is obvious that a person’s habitat should be integrated into health assessments, medical decision-making and treatment. Furthermore, he believes place is just as important as blood pressure and heart rate, especially in providing optimal care.
Increased awareness and advances in environmental health and climate change are driving geomedicine but technological advances have given the concept of linking place to medicine a boost. For instance, the rise in smartphones, the increased use in GPS tracking and data collection, the miniaturisation of electronic devices, the development of electronic health records (EHR) and the growing interest in geographic information systems in healthcare are all having an impact.
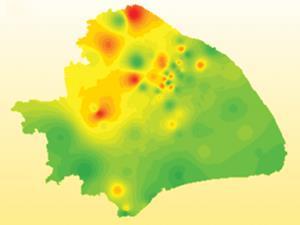
There are already instances where geographic information is being given a healthcare twist. Tech giant Google has created Google Flu, which analyses search queries such as ‘headache’ or ‘cold’ to identify flu hotspots, while a number of US agencies also use GIS, including the Agency for Toxic Substances Disease Registry to monitor environmental chemicals and the health of people who live near hazardous waste sites, and the Centers for Disease Control and Prevention for disease surveillance. Various healthcare organisations also use GIS to identify variations in healthcare delivery and access.
At an academic level, researchers are tapping into EHR data to link environmental issues with health outcomes. Brian Schwartz at Johns Hopkins Bloomberg School of Public Health in the US is one scientist linking this data. He has done numerous geomedical studies, including finding associations between obesity and the built environment and linking the proximity of antibiotic-using intensive farming operations to increased methicillin-resistant Staphylococcus aureus infection.
He says linking EHR data with other existing data provides a new opportunity to evaluate how the environment contributes to health – which is particularly important, he adds, when public health is always playing catch-up to the introduction of new synthetic chemical, energy and manufacturing processes. ‘Take fracking,’ he says. ‘It’s been done for years in this country but there was no research done beforehand.’ By linking data, Schwartz established that women who live closer to large fracking operations show an increase in pre-term births and high-risk pregnancies.
Postcode diagnostics

Integrated geographic and environmental information like this can be helpful in a healthcare setting. Broadly speaking, it can identify undiagnosed populations, highlight disease hotspots, provide early detection of new environmental health risks, predict the need for healthcare resources and ultimately pave the way for disease prevention. More specifically though, Davenhall and Berke want to see geography, public health and personal medicine converge, where a person’s postcode becomes a diagnostic tool to determine risk factors and aid diagnosis at an individual level.
A 2012 study in the American Journal of Public Health is a case in point. Researchers suggested that knowing the home address and socioeconomic data of a child could be used to predict which children with asthma were at greater risk of re-hospitalisation. The data would act as a vital sign at admission to trigger an enhanced clinical care pathway, identifying children who may need more aggressive, targeted assessments and/or interventions. This could prevent asthma attacks and reduce disparities, according to Andrew Beck, a paediatrician at Cincinnati Children’s Hospital Medical Center in the US and lead author of the study.
Taking into account the well-established links between socioeconomic disparities and childhood asthma, the researchers geo-coded home addresses and constructed a social risk index including poverty rates and house values. The researchers found that children in the high geographic risk category were 80% more likely to be rehospitalised or to revisit A&E than children at low geographic risk. Yet, the researchers noted that this information was not included in clinical care guidelines. ‘Early identification of children at increased risk could allow additional assessments and services to be put in place prior to discharge to improve patient outcomes. It could also help to target and use scarce and overburdened hospital and community resources more efficiently,’ wrote Beck in the 2012 study.
Davenhall cites the recent case of the US town of Flint as another example where a geomedicine approach could come in handy were the data available. Here, lead from the pipes contaminated the drinking water after the city’s authorities changed the water source, causing elevated levels of the heavy metal in residents’ blood (particularly that of children) which can cause brain damage. Davenhall says were it possible to have data on the makeup of every water pipe and location and link that with the local healthcare system, then a geomedicine approach would have allowed healthcare organisations to determine which households were at risk and allow for speedier testing and health monitoring.
Air Louisville
The US city of Louisville in Kentucky is pioneering a geomedicine approach with GPS technology in its Air Louisville project. Launched in 2012, the programme uses smart asthma inhalers fitted with a sensor that detects when the inhaler is used and where. That information is compared with pollution, temperature, humidity, time of year and proximity to roads and pollution sources to identify asthma hotspots and provide information about the environmental exposures that cause attacks.
Ted Smith, chief innovation officer for the city of Louisville and executive director at the Institute for Healthy Air, Water and Soil, explains that the city was the number one spring allergy capital in the US in 2014 and one of the top 20 most challenging cities to live in with asthma because of the accumulation of small particulate air pollution. ‘We don’t want to be on the worst list, so we’re trying to reduce the significant burden of breathing disorders by taking a more comprehensive approach rather than looking at patients one at a time,’ he says.
The project is a two-pronged approach where the technology helps individuals to manage their asthma and avoid its triggers, while providing aggregate data to the authorities that can be used to improve the built and natural environment. It also takes healthcare into the community and provides continuous engagement, Smith says.
We’re trying to reduce the significant burden of breathing disorders
Ted Smith
The results are impressive – a 50% reduction in uncontrolled asthma and emergency admissions for those in the project. One patient was able to pinpoint a new allergen based on where their asthma attacks clustered and was able to avoid this trigger location, Smith says. ‘The standard of care is to take medication but we’re taking a different approach to the condition looking at the geographical and built environment. We see there is more benefit if we also take these non-healthcare determinants into account rather than just focus on the clinical.’
The next phase of the project is a grant of $750,000 (£510,000) from the Robert Wood Johnson Foundation to help subsidise inhalers for local employers. If found to be beneficial, the employers will take on the inhalers as part of their employment health plan. ‘The geography of health is a city-friendly concept and this concept can help cities play their role in keeping people healthy,’ says Smith.
In this sense, geomedicine is more than just a diagnostic tool. A street address could also provide knowledge about the availability of resources for treatment, such as the location of pharmacies, access to therapeutic interventions like physiotherapy or mental health, and even proximity to exercise venues and healthy eating options. ‘Such geographic specificity allows assessments of a prognosis,’ Davenhall says.
Berke agrees, noting that clinical recommendations do not occur in a vacuum as patients will follow clinician’s advice ‘in the context of the habitat in which they live’. In a 2010 article in the Journal of the American Board of Family Medicine, he wrote: ‘If we tell them to walk or bike more for exercise but their neighbourhood has no sidewalks or crosswalk markings, inadequate traffic control, poor lighting or high crime rates, how can we expect them to be more physically active?’
Data setbacks
There are, of course, challenges with geomedicine. In the Air Louisville project, for instance, there was some resistance from the healthcare community who were doubtful of the project’s benefits, Smith says. More broadly, acceptance by healthcare professionals for a geomedicine approach will vary. Schwartz concludes there are two main obstacles for a broad implementation of geomedicine – the first is that the most useful data isn’t being collected, and secondly, doctors don’t know how to use this new information to make clinical management decisions.

It therefore raises the question why, when a patient goes to the doctor, the clinician rarely asks about a patient’s place history, despite the fact that where they have lived, worked or holidayed may have exposed them to pollutants and disease vectors, which could be relevant to their current and future health. But there is little in the way of health-relevant geographic information available to clinicians because the dots haven’t been connected between geography, public health and personal medicine, Davenhall says.
Most research on the health impact of a place tends to be generalised at a public health level, and any environmental information that doctors can tap into ‘is often stale and not geographically specific enough to be useful to either doctor, the patient or their family’, Davenhall says. ‘The problem is not with the geospatial tools,’ he explains. ‘But the incorporation of geospatial tools into the information collection and processes that produce the patient data that is useful in the healthcare setting.’ There is an issue, however, with the accuracy of geospatial data, he adds. But he says the increased dependency on location information and consumer demand for geographical accuracy (such as Google Maps and satellite navigation) will drive improvement.
Also slowing the adoption of geomedicine is the challenge of breaking the silos of research, policy and funding for public health, environmental health and personal medicine. But both Davenhall and Schwartz believe the approach will move forward as more dots are joined between the disciplines and data is shared and analysed. ‘Smarter data use across healthcare needs some serious re-thinking,’ says Davenhall. ‘Statistics are good and useful but timely analysis of health-relevant data is clearly a new mandate that has not yet been embraced.’
There are still other issues that will need to be addressed as geomedicine develops, including privacy and data protection concerns, particularly around insurance, as well as the various challenging questions regarding the personal decisions individuals would make on where to live and work based on this new health-relevant data. There are also broader issues in relation to big business around environmental data transparency and corporate responsibility. As Schwartz says, maintaining a balance between environmental and public health without putting an undue burden on industry will be a struggle.
There is certainly an appetite for this geomedicine-type information, and the small-scale applications highlight the possibilities. Interest in geomedicine is expected to grow as technology advances, and as environmental health issues continue in the media spotlight. Fundamentally, linking the environment of a place with personal medical information is a smarter way to help improve health outcomes. It’s just a matter of joining all the dots.
Katrina Megget is a science writer based in London, UK











No comments yet