Keeping cell therapy under wraps
Materials to safely encapsulate transplanted cells for could enable a revolution in the treatment of diabetes and a wide range of other diseases. James Mitchell Crow reports
Few medical discoveries have the lasting impact of the discovery made by a small multidisciplinary research team in Toronto, Canada, one hundred years ago this month. In November 1921, the team isolated a substance from the pancreas that could bring the blood sugar levels under control. By May 1922 Eli Lilly had begun insulin mass production of the substance – named insulin.
Even with the latest insulin pump technologies, T1D patient glucose levels are imperfectly controlled. Over the long term, blood sugar fluctuations put people with diabetes at elevated risk of health conditions ranging from sight loss to chronic foot ulcers. Insulin injection technologies simply can’t match the responsiveness, efficiency, and accuracy with which pancreatic islet cells release insulin to keep blood sugar levels tightly regulated.
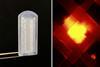
So a growing number of scientists are turning to the cells themselves, developing materials-based strategies to enable the implant of functioning islet cells for the ultimate long-term control of the condition. If these strategies prove to be safe and effective, then people with a wide range of other health conditions, from osteoporosis to cancer, could also be set to benefit.