Psychedelic drugs show promise in treating conditions including post-traumatic stress disorder and Alzheimer's. Karen Harries-Rees uncovers the come-back of medicinal hallucinogens
Psychedelic drugs show promise in treating conditions including post-traumatic stress disorder and Alzheimer’s. Karen Harries-Rees uncovers the come-back of medicinal hallucinogens
Forty years ago, Timothy Leary invited a generation to ’turn on, tune in, drop out’. But the backlash against an LSD-using youth subculture led to it becoming impossible to gain approval for LSD (lysergic acid diethylamide-25) research, which has been stalled for the last 35 years.
’It’s difficult to prove that studies are in the public interest and can be completed without undue risk to participants - and without harming the public image of collaborators,’ says John Halpern, assistant professor of psychiatry at McLean Hospital, Harvard Medical School in the US. ’But when it comes to patients suffering from debilitating illness, surely our society can find room to explore even the most unlikely of drugs as potential therapies.’
This exploration is finally happening - several studies involving psychedelics and humans have been approved in recent years. A few organisations have been instrumental in pushing this research forward: the Beckley Foundation in the UK, an independent trust that funds work to advance the understanding of how the human brain functions and the nature of consciousness; the Heffter Research Institute in the US, which supports and promotes investigation into the medical uses of psychedelic hallucinogens; and the Multidisciplinary Association for Psychedelic Studies (Maps), also in the US.
Flying the psychedelic flag
Maps describes itself as a non-profit pharmaceutical company. It focuses on the development of beneficial, socially sanctioned uses of psychedelic drugs and marijuana - helping researchers get approval for studies and funding many of them. It supports research on MDMA, or ecstasy (3,4-methylenedioxymethamphetamine) with the aim of it becoming available on prescription. This will be a long process, but the precedent has already been set. ’In the US we have found room to accept that drugs that are dangerous "on the street" may still be medicines approved for prescription,’ says Halpern. Drugs such as cocaine, methamphetamine, tincture of opium and gamma-hydroxybutyrate (GHB) are currently legal to prescribe for specific conditions. But Maps president Rick Doblin estimates that it could take five to 10 years for MDMA to become a prescription medicine.
Psychedelics have a long history of use, starting in the late 1800s, before government agencies around the world put a stop to research in the early 1970s. LSD was discovered in 1938, and used in research and therapy from the late 1940s (see Chemistry World, January 2006, p30), with the CIA in the US assessing it as a potential mind control drug during the 1950s and 1960s.
By the mid-1950s, LSD research was under way in the US, Switzerland, Germany, Italy, France, Czechoslovakia, Canada and several Scandinavian countries. Psychedelics showed the potential to treat conditions that elude drug treatment to this day, such as alcoholism, pain and anxiety in cancer patients, and post-traumatic stress disorder (PTSD).
Going underground
Then things began to change. By the mid-1960s, LSD and other psychedelics were being used as recreational drugs, triggering a regulatory backlash. In 1965, a law was passed in the US making it illegal to manufacture, compound, process or sell any hallucinogenic drugs. Medical research was eligible for a permit excluding it from the ban but in practice, the US Food and Drug Administration (FDA) asked most researchers to stop their work and return any LSD being used in their labs. In 1970, the US classified most psychedelics as schedule 1 drugs, meaning that they had a high potential for abuse and no recognised medical use. Funding dwindled and, by the early 1970s, psychedelic research had stopped.
After 1975, only three European studies of psychedelics for human use were allowed to continue, says Doblin, one in Germany and two in the Netherlands. Both of the Netherlands studies used LSD - one to treat neurotic patients and the other, conducted by Jan Bastiaans, professor of psychiatry at the University of Leiden, giving low to moderate doses of the drug to a small number of concentration camp survivors.
Just as research into LSD and other psychedelics stopped and the drugs were criminalised, MDMA arrived on the scene. It was legal and similar to MDA (3,4-methylenedioxyamphetamine), a schedule 1 drug that had shown promise during the 1960s and early 1970s for use in psychotherapy.
According to Doblin, MDMA was considered to have remarkable therapeutic potential due to its relatively short and gentle action and the lack of major perceptual and cognitive alterations, that in other psychedelics can contribute to panic attacks and bad trips.
’Many studies describe that MDMA can reduce stress, increase positive sense of self, increase sense of compassion for self and others and reduce fear of discussing highly charged psychological material,’ adds Halpern.
But by the early 1980s, MDMA too had found its way underground and become a recreational drug so, once again, regulatory agencies moved to criminalise it. In 1985 it too became a schedule 1 drug in the US - putting an end to its use in psychotherapy. Applications for studies involving psychedelics were put on hold. In Switzerland between 1988 and 1993, LSD and MDMA-assisted psychotherapy was still permitted, but, with the focus on treatment - no research was carried out. In the early 1990s, attitudes within the FDA began to change. ’The position changed to what it probably should have been in the first place,’ says Dave Nichols, professor of medicinal chemistry and molecular pharmacology at Purdue University, US, and founding president of the Heffter Research Institute. The FDA began to trust researchers - if protocols were well designed and the investigators qualified, there was no reason why the study shouldn’t be approved. The FDA still maintains this approach.
As a result, approvals are now steadily trickling through. MDMA research is the most advanced and the consensus among researchers is that there is less of a taboo surrounding MDMA than LSD. Phase I studies, in which MDMA was given to normal volunteers to measure physiological effects and pharmacokinetics, have been carried out in the US and Europe. There are now four Phase II pilot trials underway looking into how MDMA could help those with PTSD and anxiety related to advanced-stage cancer. Maps is behind all of these studies and plans to use the results to design two large multi-site Phase III trials.
Combating trauma
The first Phase II trial to get the go-ahead was in Spain in 2000, looking at the potential of MDMA-assisted psychotherapy for women with chronic PTSD following sexual assault. Mounting political pressure meant that it was stopped in 2002, after just six of the 20 patients were treated. Trial leader Jose Carlos Bouso, psychologist and psychotherapist at the Autonomous University of Madrid in Spain, says the trial showed that low doses of MDMA alongside psychotherapy was safe and that the drug showed promise in reducing PTSD symptoms.
In March 2004, the first Phase II trial to be approved in the US began. This trial, being carried out by psychiatrist Michael Mithoefer at his Charleston, South Carolina, clinic, is studying 20 patients with treatment resistant PTSD resulting from sexual or criminal assault, or from combat. The participants are patients who have already tried psychotherapy and an SSRI (selective serotonin reuptake inhibitor) antidepressant but continue to suffer symptoms.
The trial has one more year to run but Mithoefer says the results are already very promising. ’We can’t draw any firm conclusions before the study is completed but it seems extremely likely that our results will warrant the approval of larger Phase III trials,’ he says. Following this trial, he wants to start a small Phase I study of psychologically healthy people who have medical conditions such as hepatitis C, well controlled hypertension and HIV to see if they could be included in a Phase III trial. He then hopes to carry out a large, multicentre Phase III trial in the US.
In Israel, a Maps-sponsored pilot study of MDMA use in war and terrorism-related PTSD is being carried out by Moshe Kotler, a former chief psychiatrist for the Israeli defence forces who is now based at the department of psychiatry at the Sackler School of Medicine, Tel Aviv University.
Peter Oehen began studying MDMA and PTSD in Switzerland in September last year and hopes to finish at the end of next year. His study is co-sponsored by Maps and the Swiss Medical Association for Psycholytic Therapy. Oehen, a psychiatrist and psychotherapist, is getting similar results to Mithoefer, and is confident that MDMA will prove a safe and efficient adjunct to the psychotherapy of PTSD.
Tentative steps
MDMA is also being studied for its potential in treating anxiety. Harvard Medical School’s Halpern gained final approval in January this year to study MDMA-assisted psychotherapy for patients with anxiety related to advanced-stage cancer.
Should MDMA prove helpful in reducing anxiety associated with cancer diagnosis, Halpern thinks it could also help decrease the use of benzodiazepines and opiates for anxiety and pain control, which have unpleasant side-effects. ’Benzodiazepines are known to over sedate, cause coordination problems, and are also associated with cognitive problems such as verbal memory deficits,’ he says.
This is a small study and any trends need to be interpreted with caution. But if it shows that there could be significant benefits and that MDMA can be administered safely, Halpern plans to design a second, larger pilot study. ’We hope this experimental therapy might help a person face their issues and find new strength to attempt resolution and acceptance,’ he says.
Doblin believes that due to its gentle, yet profound effects, MDMA is likely to be integrated into psychiatry before other, more powerful, longer-lasting and more psychologically challenging psychedelics such as LSD and psilocybin.
Hopeful early results have stimulated speculation about the other circumstances in which these drugs could provide benefit. Eating disorders could be one field worth investigating, says Oehen, since current treatments are so ineffective. In addition, the Beckley Foundation is planning to look into the use of MDMA in psychotherapy for couples in troubled relationships.
Tuning in again
The Beckley Foundation has also gained the first approval for human studies using LSD, for a US-based study to look at dose-related changes in consciousness using electroencephalography (EEG). A second phase of this study will use magnetoencephalography (MEG) to map changes in brain activity and will also investigate the effects of LSD on creativity by measuring insightful problem solving and visualisation in relation to other cognitive functions.

Amanda Feilding, director of the Beckley Foundation, says this is a very early study but it ’opens the door to future research’. She is wary of derailing the research and will not reveal the locations of the work. Nichols is also cautious about LSD studies. ’Everyone needs to tread carefully and do these studies for the right reasons, not to make a political splash, which is the motivation at least in some cases. There is so much of a stigma, if anything goes wrong with a study it will hit the headlines,’ he says.
Feilding is discussing three further projects with institutions in the UK and Europe. One will look at the pharmacology of LSD in relation to another closely related, but non-hallucinogenic compound, lisuride. Comparing fMRI (functional magnetic resonance imaging) scans, using the two compounds, will indicate where in the brain LSD elicits its hallucinogenic effects.
MRI will also be used to investigate the psychopharmacology underlying the effects of LSD and the changes in blood flow around the brain. Feilding is particularly interested in the hypothesis that the changes in consciousness associated with psychedelics are closely linked to an increased supply of blood to the brain, enabling billions more brain cells to function simultaneously. ’We are beginning to see through our studies of Alzheimer’s disease that it is accompanied by diminished blood supply in certain parts of the brain, as is depression,’ she says. ’If LSD creates greater profusion [blood flow], it could be very useful at a sub-hallucinogenic dose to improve cerebral circulation.’
The first therapeutic trial was given approval in July. Peter Gasser, psychiatrist, psychotherapist and president of the Swiss Medical Association for Psycholytic Therapy, aims to discover if patients with anxiety related to advanced-stage illnesses can safely be given LSD-assisted psychotherapy and whether it improves their anxiety symptoms. He hopes to start the trial by the end of this year and is currently waiting for approval from SwissMedic, the Swiss drug regulation authority.
LSD, along with psilocybin, is also being studied for its potential to treat cluster headaches. In the 1950s, several research studies commented that LSD reduced migraine headaches but no clinical research has been carried out for cluster headaches. Halpern is designing a trial and hopes to put it forward to a review board later this year, with the aim of starting the trial in 2008. He and his colleagues published a case series of people with cluster headaches who had used psilocybin or LSD to treat their condition. ’Most people reported remission extension - in other words, the period of time between the cycles of attacks of episodic cluster headache was increased,’ he says. Patients also reported termination of an individual headache or cluster series. ’No approved standard medications offer the same benefit. If this research confirms these reports, it will be remarkable.’
Psilocybin is also being studied for its potential to treat obsessive compulsive disorder (OCD). Francisco Moreno, associate professor of psychiatry at the University of Arizona, US, has completed the first FDA-approved study in more than 25 years to examine the use of psilocybin in a patient population. The investigators studied 10 patients suffering from OCD and found psilocybin reduced their symptoms, replicating the findings from patients in case studies.
Meanwhile, Charles Grob, professor of psychiatry and biobehavioural sciences at UCLA school of medicine, US, is investigating whether psilocybin might be effective in reducing anxiety, depression and physical pain in people with advanced cancer. His study started in April 2004. So far, 10 patients have been treated and one more is needed to finish the research. Two other groups in the US are carrying out similar work, but neither will release details at this early stage.
’Psychedelics are an amazing category of substances,’ says Feilding. ’Only by understanding the scientific neural and physiological correlates of what is happening underneath the experience will we more easily be able to explain why they could be therapeutic.’
Research is already altering the perception of psychedelics - enabling them to come out of the underground and be viewed as possible treatments. In less than 10 years time, patients with a series of distressing disorders for which current treatments fall far short, could be receiving psychedelics on prescription. Leary may have been an unwitting advocate of a psychiatric wonder drug.
Karen Harries-Rees is a science journalist based in Melbourne, Australia
Further Reading
Maps
Beckley Foundation
Heffter Research Institute
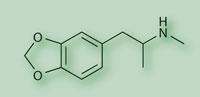
MDMA , 3,4-methylenedioxymethamphetamine, also known as ecstasy, is a ring-substituted phenylisopropylamine derivative. It is a psychoactive drug chemically similar to the stimulant methamphetamine and the hallucinogen mescaline. It was initially patented by Merck in 1912 as an intermediary chemical used in the synthesis of hydrastinine. It was rediscovered by chemist Alexander Shulgin in the 1970s. Some researchers say that MDMA should be in a separate drug class, the entactogens or empathogens. These reduce fear associated with emotionally upsetting thoughts, feelings or memories and generate or enhance feelings of closeness to others. The effects of MDMA include feelings of openness, euphoria, empathy, love and heightened self-awareness, lasting for three to five hours.
LSD, or lysergic acid diethylamide-25 was first synthesised by Albert Hofmann in 1938. It is a chiral compound with two stereocentres at the carbon atoms C-5 and C-8, so four optical isomers of LSD could exist. The C-5 isomers of lysergamides do not exist in nature and are not formed during synthesis from d-lysergic acid. Of the two C-8 isomers, only one (the d-) LSD is psychoactive. LSD is one of the most potent mind-altering chemicals known. The current theory is that it works by inhibiting serotonin. Its effects are very variable, are strongly dependent on the setting and usually last for eight to 12 hours. It alters perception, mood and psychological processes.
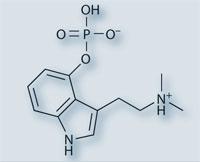
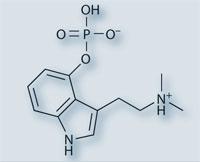
Psilocybin, along with psilocin, is the primary active ingredient of psilocybe mushrooms and are equally psychoactive. The ratio of psilocybin to psilocin varies between species. Psilocin, the dephosphorylated free base alcohol of psilocybin, is unstable and breaks down when the mushroom is dried, whereas psilocybin lasts much longer. They are part of the tryptamine family and closely resemble the neurotransmitter serotonin. Like LSD, they are thought to inhibit serotonin. The effects are also strongly dependent on the setting and are similar to LSD.










No comments yet