Scientific and digital collaboration is key to maintaining the UK’s esteemed status in global life sciences and pharma circles. CPI exists to facilitate and underpin those vital relationships
Innovation can be defined as the art or science of converting existing inventions and ideas into practical products or processes, and it is thriving in the UK. In spite of the uncertainty businesses face due to Brexit, the UK is one of the world’s five most innovative countries. This is largely due to the quality of research coming out of its world-leading universities and strong opportunities for accessing investment says 2019 study Creating Healthy Lives – The Future of Medical Innovation from Cornell University et al.
Advanced manufacturing technology and digitalisation has the power to reduce pharma innovation costs
The life science industry is a critical part of the UK’s innovation output, which generates a turnover of over £70 billion annually according to a 2018 Office for Life Sciences report. However, with a rapidly ageing population and soaring R&D costs, pharmaceutical and healthcare providers are under pressure. For UK life science organisations to remain internationally competitive, solutions that help companies overcome the growing challenges in this sector are crucial. It will require industry, academia and government working together to understand and improve process inefficiencies throughout the clinical supply chain. By taking advantage of advanced manufacturing technology and digitalisation, the cost of pharma innovation can be reduced and the UK can remain a world leader in bringing radical treatments to market.
Efficiency is everything

With people living longer worldwide, society is seeing large increases in diabetes and age-related disease – placing significant strain on healthcare systems. To effectively manage this evolving healthcare landscape, there is a demand for improved access to personalised medicine, gene therapies and other biologics. However, innovative new forms of treatments come with exorbitant development costs. Taking clinical attrition into account, the price tag on the development of new drugs currently stands at around 10 years and £2 billion, and is rising rapidly.1 That’s an unsustainable trajectory and intensive work is required to identify how time and money can be saved.
Collaborations offer a wealth of new and diverse technology, and the expertise to develop new industrial processes
The inherent inefficiency of drug manufacturing is one factor to investigate because batch processes are not conducive to producing small quantities of tailored, patient-centric formulations. They are also inflexible to fluctuations in demand.
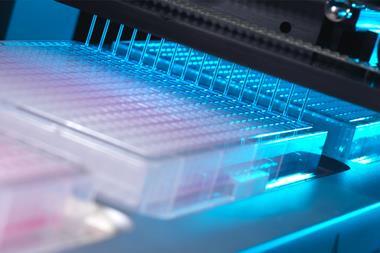
Highly customisable continuous manufacturing methods, by which drugs can be produced quickly and reliably when needed, can help address these problems. Digitalised manufacturing processes could also increase supply chain efficiency. Transferring laboratory experiments to a computer can significantly reduce the use of raw materials. And real-time data collection with process analytical technology (PAT) will enable more rapid decision-making throughout the manufacturing process.
Greater than the sum of its parts
The challenge of integrating new technologies and reducing waste in pharmaceutical development is too complex to be overcome by the heavily siloed and fiercely competitive R&D models that typified big pharma in the 1980s and 1990s. The industry has recognised that collaboration is key to facilitating and implementing innovative ideas that positively impact patients’ lives. Collaboration gives companies access to a wealth of new and diverse technology, as well as expertise that can assist in the development of new industrial processes. Frequently, life science industry collaborations are research partnerships between big pharma and small biotech companies that happen through the establishment of bioscience clusters or open-innovation approaches. According to research from HBM Partners, two thirds of newly approved drugs currently originate from either academia or small biopharma companies, and big pharma is eager to access this source of external innovation. These innovation models are taking up an increasingly large percentage of R&D budgets. However, the full potential of collaboration can only be unlocked when big pharma begins to work hand in hand not only with academia and SMEs, but also with each other.
Large-scale collaborations between government, industry and academia will usher in the pharmaceutical supply chain of the future
The Medicines Manufacturing Innovation Centre under development near Glasgow is taking a three-pronged approach to collaboration by bringing together industry, academia and government. Crucially, it represents the first time that two of the UK’s leading pharma companies, GSK and AstraZeneca, have worked together to co-develop new technologies. As the centre’s academic partner, the University of Strathclyde will provide front-line research and methodologies in manufacturing technology. With input from across the supply chain, the centre aims to develop new processes that ensure that the UK can establish itself as a leader in fine chemical and small molecule manufacturing. Once completed, this collaborative centre will provide companies – both small and large – with access to technologies that enhance manufacturing efficiency in a GMP-capable environment. Ultimately, it will allow new drugs to be brought to market more quickly and at reduced cost.
Designing disruption

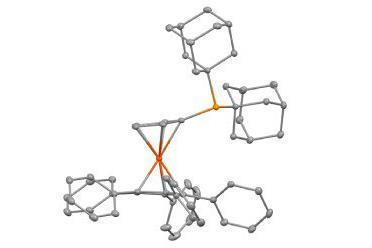
The Medicines Manufacturing Innovation Centre is currently working towards two government-financed grand challenges designed to solve the most prominent manufacturing problems highlighted by industry. Both projects aim to increase supply chain efficiency and reduce the waste and costs associated with pharmaceutical manufacture. This work has the potential to enhance the UK’s access to a global fine chemicals market worth almost £100 billion.
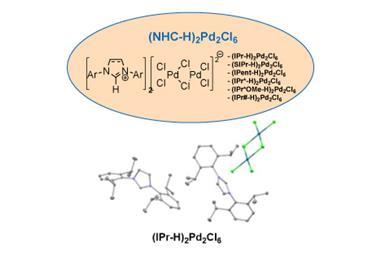
Grand challenge 1
This focuses on developing a new PAT-enabled platform for manufacturing oral solid drug formulations with continuous direct compression. This technology enables much finer process control than batch methods and supports the rapid development of pharmaceutical formulations. However, it is an emerging technology with a high adoption cost. The project is currently housed within the University of Strathclyde where a digital twin of the platform is being created. This key innovation will allow for faster optimisation of continuous manufacturing processes with minimal use of expensive raw materials.
Grand challenge 2
The second challenge aims to improve supply chain efficiency by giving healthcare systems access to drug supplies as demand arises. To achieve this, consortium partners are developing a platform to enable just-in-time manufacturing for small molecule drugs. Automated technology will generate real-time quality data throughout the manufacturing process and produce drugs at quantities that meet near-term market demand. Ultimately, the project aims to develop responsive technology that can fulfil individual patient orders on demand. The combined strength of its founding partners – GSK and AstraZeneca – is pivotal to the project’s success. Their joint contribution of funding, creativity, talent and in-depth, specialist expertise is vital.
Making collaboration successful
The unique collaboration underpinning this state-of-the art manufacturing centre is a fantastic example of how different stakeholders in the pharmaceutical supply chain can enable the development of new solutions to complex manufacturing problems. It also demonstrates how industry competitors can add value by identifying common ground to explore in partnership. Without carefully balancing the needs of all parties, collaboration involving many different viewpoints easily comes unstuck. It is therefore crucial that the partners interact often and communicate openly to discuss progress to ensure individual objectives are met. The centre recently brought its contributing partners together to share their perspectives and map the project’s future. They discussed new manufacturing challenges to be tackled in future grand challenges. Maintaining the close involvement of all partners helps to ensure that the centre will be a major asset across the life science supply chain.
Large-scale collaborations between partners representing government, industry and academia will usher in the pharmaceutical supply chain of the future – one that is agile and responsive to the evolving demands of healthcare systems. By embracing this collaborative mentality with projects like the Medicines Manufacturing Innovation Centre, the UK life science industry can retain its leading position among global innovators and lower the cost of pharmaceutical R&D. Patient access to personalised, safe and effective new therapies is sure to follow.

Dave Tudor is the managing director of the Medicines Manufacturing Innovation Centre
The Medicines Manufacturing Innovation Centre is a collaboration between CPI, University of Strathclyde, UKRI, Scottish Enterprise and founding industry partners, AstraZeneca and GSK.
References
1. J A DiMasi et al,J. Health Econ., 2016, 47, 20 (DOI: 10.1016/j.jhealeco.2016.01.012)














No comments yet