This series of Chemistry World reports is part of a forth coming e-book and hardback to be published by the Royal Society of Chemistry. The book was motivated by a desire on the part of the editors and the authors to produce a body of information on the new and deadly coronavirus about which the world was largely uninformed and for which it was totally unprepared.
Our hope and our goal in producing this book is that scientific knowledge will enable us to survive this pandemic and to be better prepared for future viral epidemics and pandemics. These articles are dedicated to those who lost their lives to COVID-19, and to the health care workers who valiantly tried to save them, as well as to the scientists who worked in the field to develop new test methods, pharmaceuticals, and vaccines.
Our perception is that few Western scientists or non-scientists took much note of the either the 2003 outbreak of Severe Acute Respiratory Syndrome coronavirus (SARS-CoV) in China, or the 2012 outbreak of Middle East Respiratory Syndrome coronavirus (MERS-CoV) in Saudi Arabia. Both viruses spread to about 30 countries, and each killed between 800 and 900 people - with mortality rates of 10% and 35%, respectively. By contrast, with a lower mortality rate, estimated at 3-5%, SARS-CoV-2 spread around the globe in just four months, and in less than eight months killed more than one million people, still counting. Those countries that immediately began lockdown, testing, and contact tracing were able to contain the virus; those that did not continue to experience large numbers of hospitalisations and deaths.
Here are the facts: The first case of SARS emerged in Guangdong Province, China, in November 2002. SARS-CoV was identified in 2003 and spread to 32 countries or regions, primarily in mainland China, but also Hong Kong, Taiwan, Singapore, Vietnam, and Canada. There were 8437 reported cases of SARS and 813 deaths reported to the World Health Organization (WHO). The first case of MERS was reported in 2012 in Saudi Arabia. Since then, 27 countries have reported cases, although 80% were in Saudi Arabia. From September 2012, until the end of November 2019 and now, WHO has been notified of 2494 confirmed cases of MERS and 858 deaths.
Transmission of SARS-CoV is person-to person through unprotected contact, while MERS is transmitted via dromedary camels or infected people (WHO 2019). Although there are gross similarities in the clinical spectra of SARS, MERS and COVID-19, the new viral disease is far more contagious and dangerous than its predecessors. In part because SARS and MERS were more deadly than COVID-19, they have all but disappeared. However, the morbidities suffered from COVID-19 infections are more pervasive and more persistent than in the case of SARS or MERS, and people afflicted with moderate to severe cases of COVID-19 are more likely to suffer chronic debilitation.
Like MERS-CoV, the clinical spectrum of SARS-CoV-2 infection ranges from no symptoms (asymptomatic) or mild respiratory symptoms to severe acute respiratory disease and death. A typical presentation of MERS involves fever, cough, and shortness of breath. Pneumonia is a common finding, but not always present. Gastrointestinal symptoms, including diarrhea, have also been reported. Both with MERS and COVID-19 severe illness can cause respiratory failure that requires mechanical ventilation and life support in an intensive care unit. Both viruses appear to cause more severe disease in older people, people with weakened immune systems, and those with chronic diseases such as renal disease, cancer, chronic lung disease, and diabetes.
Like SARS-CoV, transmission of SARS-CoV-2 is primarily from person to person. However, according to the World Health Organization (WHO 2020), SARS-CoV transmission appears to occur mainly during the second week of illness, which corresponds to the peak of virus excretion in respiratory secretions and stool, and when hospitalised patients with severe disease start to deteriorate clinically. Symptoms are readily apparent including fever, cough, and shortness of breath, which facilitate detection and hospitalisation. Many cases of human-to-human transmission of SARS-CoV have occurred in a health care setting in the absence of adequate infection control precautions.
Transmission of SARS-CoV-2 is altogether different in that pre-symptomatic or asymptomatic individuals can shed and transmit the virus within days of infection, and well before the onset of symptoms. In fact, viral infection, reproduction, and shedding occur entirely without symptoms in a large percentage of patients who test positive for SARS-CoV-2. This alteration in the pattern of disease transmission may relate to the acquisition of the furin cleavage site in the spike protein and/or increased binding affinity for ACE2 in the case of SARS-CoV-2 as compared with SARS-CoV.
COVID-19 can progress in severity from mild to moderate to severe, sometimes with a precipitous drop in oxygen saturation in severe cases such that mechanical ventilatory life support is required. This is can be because the virus is equipped to circumvent the immune system such that a cytokine storm, in which cells release massive quantities of small proteins called cytokines, results in extensive tissue damage with dysfunctional coagulation and multi-organ failure. Cytokine storm is a component of the respiratory diseases caused by SARS and MERS as well as by COVID-19 and is particularly detrimental to patients with comorbidities such as hypertension, diabetes, and cardiovascular disease.
The main threat of SARS-CoV-2 is its propensity to be spread by unknowing asymptomatic carriers in exhaled aerosols containing their respiratory droplets. In fact, this attribute presents the greatest challenge to effective public and global health management, since the virus can survive for hours as indoor aerosols and on non-porous surfaces. Social distancing, mask wearing, hand washing, and disinfection are effective tools in slowing the spread of the virus, but gatherings of large numbers of people are to be avoided until community spread is contained.
The initial series of eleven Chemistry World reports chronicled the outbreak of the novel coronavirus (SARS-CoV-2), beginning with the first known disease case in China on 1 December 2019; it described what had been learned and practiced during the first six months after the declaration of the COVID-19 Pandemic on 11 March 2020. While the world awaited a safe and efficacious vaccine many efforts were undertaken to find suitable pharmaceutical therapies and appropriate patient management interventions.
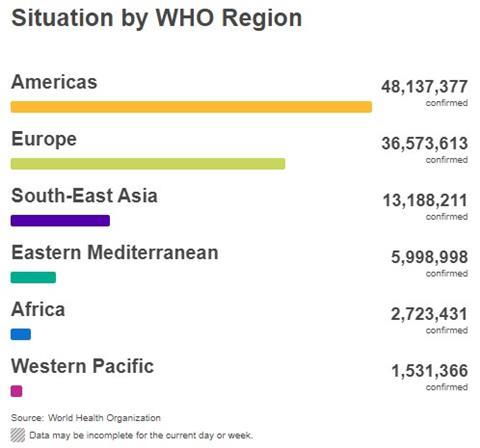
This second release, consisting of 19 reports, continues to document our progress in fighting COVID-19 during the second six months of the pandemic. The e-book and hardback is planned to be released at the conclusion of the third six months. The book will include additional updates and new information that becomes available as well as recommendations for the future. As of 15 February 2021, according to the WHO there have been 108,153,741 confirmed cases of COVID-19 and 2,381,295 deaths (an overall 2.20% case fatality ratio). We noted earlier that SARS-CoV-2 had killed more a million people in just under eight months. Here we are after four more months and well over twice as many people are dead. The regional breakout of confirmed cases is illustrated in the bar graph below (figure 1).
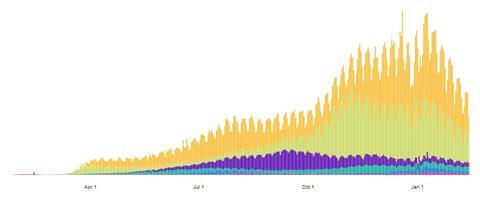
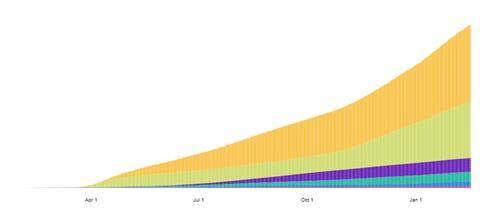
As may be seen in the histograms below, also for 15 February 2021, the number of cases in every region is on the decline (figure 2), however cumulative death numbers (figure 3) are staggering (2,381,295 total deaths). Colours on the histogram plots correspond to WHO Regions as indicated on the previous bar graph.
“No one is protected until everyone is protected,” said Dr. Tedros Adhanom Ghebreyesus, the Director General of the WHO, early in the pandemic. All WHO Regions, except for South-East Asia where the pandemic began, had faced increasing infections and deaths from COVID-19 from 11 March until the end of 2020. The US led the world in infections and hospitalizations in part because of failure to implement appropriate control measures and take actions to test and trace quickly enough to mitigate the spread of the virus. Early in the pandemic, it became clear that the longer any country waits to do so the greater will be the difficulty, economic cost, and number of lives lost. We include with this release “country reports” from New Zealand, Turkey, and Sweden, each of which has dealt with the pandemic differently.
After a year of fighting to slow the global spread of SARS-CoV-2, the scientific and public health communities have learned a great deal. As of 15 February 2021, lifesaving vaccines have been delivered to vaccination sites in many parts of the world. While the development of these vaccines has taken place in record time, the virus has continued to win the race to infect as many people as possible. Furthermore, our early concern that viral mutation would be a major problem has been realized. When specific mutations, or sets of mutations, are selected through several rounds of viral replication new variants can emerge. Since the beginning of 2021, dangerous variants have been detected in the UK, South Africa, Brazil, and California. These variants are more easily transmitted such that they can easily become dominant elsewhere.
From the beginning of the pandemic, vaccine development, testing, manufacture, and distribution has been an international priority, and this has worked well in much of the developed world. Indeed, it is encouraging that more than 240 COVID-19 vaccines are in various stages of development globally. In this Chemistry World release we feature a detailed report on vaccination and vaccines that describes eight vaccines that are currently being distributed and administered in various countries. Very few individuals that have been vaccinated thus far in the US and UK have had serious side effects. However, vaccination has not happened rapidly enough in most countries to mitigate the spread of SARS-CoV-2. And, unfortunately, poorer countries are not able to afford the costs of mass vaccination on their own.
It should be noted that because of inadequacies in GIS-based sequencing, it has not been possible to monitor the emergence and translocation of SARS-CoV-2 variants in real time. Furthermore, if we do not completely understand the import of mutational changes in the variant viral genome, and how it interacts with the host genome, we cannot know precisely how to mitigate its spread by vaccination. It now appears that vaccines will need to be modified relatively frequently, and “boosters” will be required to maintain immunity against SARS-CoV-2 variants. These topics will be dealt with in the e-book and hard back as our knowledge is currently incomplete.
Already, however, we can say that international surveillance and testing of SARS-CoV-2 variants could be greatly improved by the sharing of validated, variant-specific assays. Similarly, a central repository of sera and cells from individuals with past infection, with or without past COVID-19 immunization, could facilitate testing of seroneutralisation and cellular immunity against newly discovered variants. Importantly, global access, availability, and affordability of COVID-19 vaccines that work is necessary to ensure that no country or population is left behind.
There is significant concern whether vaccines will be available timely, and whether they alone will be adequate to save endangered lives around the world. Vaccines induce a natural immune response by exposing the body to a weakened, dead or replica virus. Another class of therapeutics, monoclonal antibody preparations, can provide immediate protection when infused directly into the body. With increasing production and availability, these preparations could be administered at infusion centres to high-risk patients in early stages of COVID-19 infection.
Pharmaceuticals can offer an addition line of defence against the virus. Again, there are economic disparities in the ability of countries, and certain populations within countries, to afford newly developed drugs or costly monoclonal antibodies. For this reason, and because of the protracted time course necessary for development and testing of new drugs and other therapies, repurposed drugs have been investigated by scientists internationally to provide ready treatments for persons and families who may become infected with SARS-CoV-2.
At the beginning of the pandemic there were few drugs specific to the coronavirus in the pipeline. Drug repurposing efforts have not been well funded, but many candidates have been found and pre-clinical investigations as well as clinical trials have been initiated. Some candidate repurposed drugs that have proven records of safety and indications of efficacy have been widely used in countries where there is a critical need for antiviral agents. Several reports in this release bear on the issue, including detailed coverage of candidate pharmaceuticals in in silico screening and animal-alternative model systems. A final chapter on pharmacotherapies will be available in the forthcoming e-book and hardback.
Although several repurposed drugs are promising and available globally, none should be used without a medical prescription, nor at dosages above those recommended. In the meantime, public health policies regarding prevention, biosafety measures, large-scale testing, and adequate epidemiological surveillance must be followed assiduously. The bottom line is that all available approved vaccines, pharmaceutical interventions, public health methods, clinical and research approaches are needed to treat COVID-19 and to slow the global spread of SARS-CoV-2. Every effort should be made to do what is necessary to save human lives
Introduction: the coronavirus pandemic and the future
This series of Chemistry World reports is part of a forth coming e-book and hardback to be published by the Royal Society of Chemistry. The book was motivated by a desire on the part of the editors and the authors to produce a body of information on the new and ...
 Currently
reading
Currently
reading
Introduction: the coronavirus pandemic and the future
- 2
- 3
- 4
- 5
- 6
- 7
- 8
- 9
- 10
- 11
- 12
- 13
- 14
- 15
- 16
- 17
- 18
- 19
- 20
- 21
- 22
- 23
- 24
- 25
- 26
- 27
- 28
- 29
- 30
- 31
- 32
- 33
- 34
- 35
- 36
- 37
- 38
- 39
- 40
- 41
- 42