Tantalising press-released data on Biogen and Eisai’s lecanemab prompt questions without firm answers
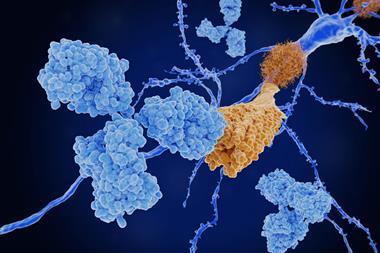
Another anti-amyloid antibody treatment for Alzheimer’s disease has hit the news this week. Eisai and Biogen have press-released top-line findings from a phase 3 trial of lecanemab. The results appear positive, showing a statistically significant slowing of cognitive decline measures over 18 months, compared with a placebo, as well as evidence that the drug reduces levels of amyloid protein in patients’ brains.

So far, so good. But as always – and particularly with slow-moving and hard-to-monitor diseases like Alzheimer’s – these top-line results will need to be backed up with strong data and rigorous analysis. Biogen and Eisai are preparing a journal publication, and will present more data at the Clinical Trials on Alzheimer’s Disease (CTAD) conference on 29 November. No doubt those revelations will be eagerly anticipated and heavily scrutinised. Until then, we should be wary of getting too excited.
On the positive side, the numbers appear to be better than those for Biogen’s previous effort in this area – Aduhelm (aducanumab). While Biogen (somewhat controversially) managed to convince US regulators to approve the drug, it was much less successful at convincing healthcare providers to actually use it.
That said, the effect on cognitive decline is still relatively modest. The Clinical Dementia Rating-Sum of Boxes measure employed in the trial is an 18-point scale that scores patients across six categories of dementia symptoms and performance. How much of a difference on this scale would translate into a meaningful difference in people’s lives depends who you ask. Some Alzheimer’s researchers have suggested it would require a 0.5–1 point difference. Others have pegged it higher, at 1–2 points difference. The scores for patients receiving lecanemab ended up, on average, 0.45 points better than the control group by the end of the 18-month trial.
There are also indications from the top-line results that lecanemab may cause fewer brain swelling and haemorrhage side effects than aducanumab. Both abnormalities detected on brain imaging, and particularly those that led to noticeable symptoms appear appreciably lower. All the numbers certainly appear to be moving in the right direction. The question is, have they moved far enough to justify the likely cost of the drug if it gains approval?
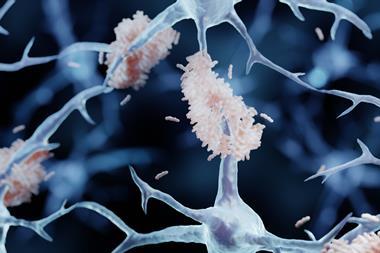
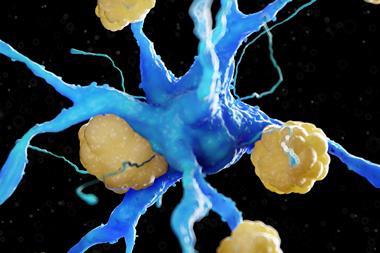
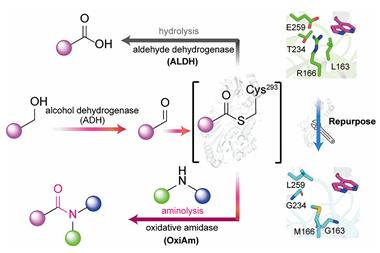
From a biochemical point of view, lecanemab binds most strongly to relatively small amyloid beta protofibrils – before they aggregate together to form the disease’s characteristic brain plaques. That’s subtly different to adacanumab and other anti-amyloid antibodies in development by Roche–Genentech and Eli Lilly, for example, which tend to bind most strongly to more aggregated forms of the misfolded protein. Whether that difference is important remains to be seen. There are suggestions that these results will prompt a revival of the ailing amyloid-driven model of Alzheimer’s. My suspicion is that that’s unlikely – one swallow does not a summer make!











No comments yet