‘Liquid biopsy’ blood test accurately spots cancer by detecting DNA methylation
Power of AI harnessed to identify 50 different cancers before symptoms have even begun to emerge
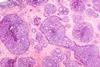
A new blood test that probes methylation sites in DNA can accurately predict whether a person has any one of 50 cancers and where the tumour is growing.
The California-based healthcare company Grail, which developed the test, owns a large database of methylation patterns in cancerous and non-cancerous cell-free DNA. From that repository, a machine learning program was developed to analyse blood samples. The algorithm identified methylation changes that are classified as cancerous or non-cancerous, and it could even pinpoint the tissue of origin before the onset of symptoms.
