Determining the role drugs and poisons may have played in death is the responsibility of forensic toxicologists. Nina Notman reports

On the evening of 27 January 2009, Lakhvinder Cheema and his fiancée Gurjeet Choough sat down to eat curry left over from the night before at Cheema’s home in Feltham, West London. Shortly after they had eaten, both started to experience pins and needles around their mouths. Their symptoms rapidly escalated to loss of sight, paralysis and copious vomiting. Upon arrival at hospital they were treated with anti-sickness drugs, but the vomiting continued unabated. Cheema’s heart started to race and then beat erratically. His blood pressure dropped, he had convulsions, and in the early hours of the morning – just two hours after arriving at the hospital – he died.
Choough’s heartbeat also became erratic and her blood pressure low. Suspecting poisoning by this point, doctors attempted to flush the poison from her body, and she was placed in a medically induced coma to aid recovery. A week later she was fully better. The medical emergency had passed, but the police were still hard at work uncovering who poisoned them, why and with what.
Out for revenge
The ‘who’ and ‘why’ proved easy to crack: Cheema’s recently spurned lover – Lakhvir Kaur Singh – had been let into the house by a tenant earlier in the day and been seen opening the fridge where the curry was stored. She was arrested within hours of his death.
The ‘what’ was harder to solve, and became one of the most challenging cases forensic toxicologist Denise Stanworth at LGC in Abingdon, UK, has worked on during her 30 year career. Poisons such as arsenic and nicotine were swiftly ruled out: the symptoms didn’t match. The team suspected plant alkaloids, but again the symptoms didn’t exactly correlate with those of any known examples.
Samples of the victims’ blood, the curry and an Indian herbal powder (found in Singh’s coat pocket and handbag) arrived at the LGC labs. Initial screens against spectral libraries of known poisons using gas chromatography–mass spectrometry (GC–MS) drew a blank. ‘We then turned to LC–MS [liquid chromatography–mass spectrometry] to look for anything that was actually present in the samples,’ says Stanworth. ‘That’s when we came up with several molecules that seemed to be related, and that had a very large molecular weight. Plant alkaloids come into that category. It’s not possible to do that by GC–MS because the molecules become fragmented and the fragments are so small that you don’t always recognise where they have come from.’ The same peaks appeared in the victims’ blood, curry sauce and the herbal powder.
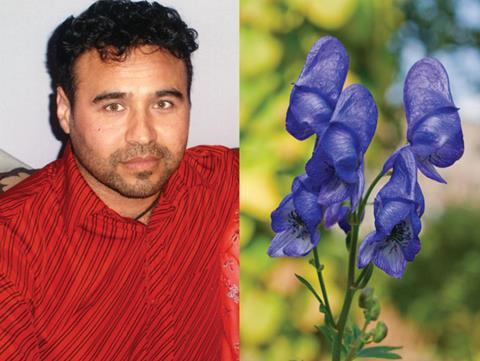
The team narrowed the search to an alkaloid from a plant in the aconite family, but their findings didn’t match any substance from the European variety. Literature searches led them to tentatively identify it as an alkaloid from Aconitum ferox, a type of aconite that grows in the Himalayas.
To backup their suspicions the team sought help from an unusual source: the scientists at the UK’s Royal Botanic Gardens in Kew. ‘Kew Gardens has its own laboratory, they have reference samples of substances from lots of different plants and reference spectra from those plants. So, they could run it and identify the samples as well,’ says Stanworth. ‘We had a bit of a belt and braces approach really, two laboratories sort of conferring with each other and both coming up with the same answer.’
Windows of detection
The most useful sample type for investigating cases of poisonings that have resulted in death is blood, explains Simon Elliott, a forensic toxicologist and the managing director of Roar Forensics in Malvern, UK. If someone has taken an overdose or ingested a poison, they are usually going to die when the levels of the poison in their blood have reached their peak, he says. If they die quickly, stomach contents can be useful too.

Blood is also used in immediately-reported cases of suspected poisonings where the victim has survived. When reporting has been delayed, urine is more useful. ‘Think of urine as a collector of your drug history,’ says Elliott. ‘Drugs can be present in the urine for days after they have been taken whereas they are typically only in the blood for a day or two at most.’
After this window of opportunity has passed, hair becomes key. ‘In rape cases [where the use of sedatives is suspected] the issue is that usually the victim won’t go to the police, a doctor or the hospital until a few days after the event,’ says Elliott. By which point the drug may have cleared from their urine, although some metabolites will hang around longer. A hair sample would be collected immediately, and then a second at least four weeks later. ‘You would analyse the two hair samples and you should see the drug in the second sampling but not the first [because it takes time for the hair to grow out of the scalp]. Think of hair as a recorder of drug history that extends as long as the hair.’
This length of detection window means hair analysis can also be used in cases of suspected long term abuse of children or vulnerable adults, particularly the elderly and those with dementia. It can show if people have been given sedative-type drugs to make them easier to control, or if prescribed medication has been withheld. Hair is also useful in post mortem situations where heroin users have accidentally overdosed as it will reveal if any changes in the levels of drug taken has occurred in recent months. ‘For instance, someone with a drug problem has just been imprisoned and hasn’t had access to drugs. They get discharged, they get out, score some heroin or something, take it and they die because they’ve lost their tolerance,’ explains Robin Braithwaite, a professor of forensic toxicology at King’s College London, UK.
Tissues can also hold a reliable record of any drugs or poisons taken or administered for a long time after a person has died. The key to convicting Harold Shipman – a doctor and the UK’s most prolific serial killer – was thigh tissue, explains Braithwaite, who was a prosecution expert witness for this case. Shipman was convicted in 2000 of injecting 15 patients with lethal doses of morphine or diamorphine, but is suspected to have killed more than 200 of his patients since the 1970s. When suspicions were aroused, some of his victims were disinterred and morphine was found in thigh muscle tissue.
Tools of the trade
The body samples analysed by forensic toxicologists are collected by pathologists, the police or doctors. Once they arrive in the lab, toxicologists have a range of analytical tools available to screen them for any evidence of drugs or organic-based poisons.
Immunoassays – which contain antibodies that bind to typical drugs of abuse – are widely used for initial screens. These assays simply give a yes or no indication of whether certain drugs are present, explains Elliott. GC–MS, the technique used first in the curry poisoning case, allows toxicologists to compare the mass spectra of samples to those of widely used drugs, poisons and their metabolites.

High performance liquid chromatography with diode array detection (HPLC-DAD) exploits molecules’ ultraviolet (UV) absorption to detect them. ‘The downside of UV is that drugs belonging to the same family could look like each other,’ says Elliott. This isn’t an insurmountable problem as more than one technique is typically used for each sample.
LC–MS, the technique that cracked the curry poisoning case, is growing in popularity. Using tandem mass spectrometry detectors (LC–MS/MS), in which each peak in the mass spectrum is further fragmented to give structural information, is more useful still. ‘That gives you the opportunity to look for a much wider variety of things,’ explains Braithwaite. ‘You can look for a wide range of polar and non-polar compounds, particularly drug metabolites. This is the big change from the days where we only had GC–MS, and there were difficulties in measuring important polar metabolites such as morphine in heroin-related deaths.’ LC–MS/MS is also very sensitive, meaning it can detect drugs – such as the often-abused pain-reliever fentanyl – that are only present in the blood at very low concentrations. Another related new and highly sensitive technique, that most forensic toxicologists now aspire to have access to, is quadrupole-time-of-flight (QTOF) LC–MS.
With some of these modern LC–MS machines it is possible to gather information on the mass of a substance with a high degree of accuracy, this helps with the identification of new or unusual drugs and their metabolites. ‘More and more, we’re turning to accurate mass as a form of LC–MS for looking for unusual substances,’ says Stanworth. Even with a dazzling array of techniques on offer, Stanworth does sometimes find herself accidentally using a significantly cheaper instrument: her nose. She worked on a case where a mother had given her children a caustic chemical to drink and then had drunk it herself: a murder–suicide. ‘There was a lot of damage internally and so we knew we were looking at a very caustic chemical,’ she explains. The lab was sent stomach contents of the victims and asked to identify it. ‘I knew it was phenol because as soon as I opened the bag I could smell it.’
Outside the norm
‘It’s much easier now, you can look for almost everything,’ Braithwaite says, referring to highly sensitive instruments now available. ‘The only caveat there is you’re assuming that it’s a drug poison [an organic molecule] when actually, in some cases, there may be other types of poison such as a metalloid or a metal.’ Inductively coupled plasma mass spectrometry (ICP-MS) is typically used when searching for these types of poisons that include arsenic, mercury and thallium.
And when the sample being tested isn’t from a person, but instead the drink or foodstuff that they ingested – or nearly ingested – different techniques are needed. ‘I’ve had cases where antifreeze has been put in cooking oil, slug pellets have been put in someone’s curry and bleach has been added to soft drinks,’ says Stanworth. ‘We go back to the old fashioned wet chemistry in a lot of those cases.’ The pH of the sample can show when a strong acid or alkali has been added, colour tests indicate oxidising agents and toxic anions can also be tested for. Chlorate, for example, is present in many household poisons such as bleach and some weedkillers.
Once the laboratory tests are complete, the forensic toxicologist who directed the analysis will report the findings to whoever commissioned the work. This is normally the police for criminal cases, and the coroner when the cause of death was sudden or unexpected, but not suspicious (such as drug overdoses).
Forensic toxicologists can be called to present their evidence in court. In the criminal (crown) court they may also have to defend their findings or act as expert witnesses for the defence. ‘The defence like to pick through things that you have said and see if they can perhaps try and throw up other possibilities in your interpretation and perhaps confuse the jury – we call it “muddying the waters”.’ In the poisoned curry case, the evidence Stanworth’s team collected – together with the scientists at Kew Gardens – helped convict Singh of murder. She was sentenced to serve a minimum of 23 years in prison.
International variations
In the UK, forensic toxicology for the criminal courts is largely carried out by a handful of private companies including LGC and Roar Forensics. Some in-house police labs do some simple screening. A larger number of private firms, NHS hospital toxicology and some university labs do work for the coroner’s courts (known as post-mortem toxicology) and family courts. ‘The situation across the whole UK regarding forensic science, including toxicology, is a real dog’s breakfast,’ says Robin Braithwaite of King’s College London, UK.

However, the quality of forensic toxicology in the UK has, on the whole, been rising in recent years. This is partly because laboratory accreditation and stricter quality standards have been introduced. Better funding for labs has also contributed. ‘In its latter days, the Forensic Science Service [which closed in 2012] was very poorly funded and lacked investment for introducing new technology – particularly LC–MS.’ These days, most of the larger commercial toxicology labs are very well funded, he says. ‘But fierce competition between laboratories in both the NHS and private sector has potential risks, particularly regarding quality standards’.
‘Another important issue that gets little attention is that there is little incentive for commercial forensic laboratories or NHS labs to undertake research.’ This means the field is not advancing as fast as it could, and the use of unusual poisons or new designer drugs could be missed.
By contrast, in Germany, university laboratories dominate the forensic toxicology sector, explains Stefan Toennes, head of forensic toxicology at the Institute of Legal Medicine, University of Frankfurt. This means that research is conducted alongside case work for the police and coroners. In Germany there are also in-house police labs that do non-biological samples such as determining the purity of seized drugs, and also a few private firms who do routine work such as abstinence controls, says Toennes. ‘However, everything that is more complex or specialised is done by the universities.’ He adds that the universities’ independence from the prosecutors, for example compared to carrying out forensic toxicology in police labs, is a big positive of the German system. ‘This is a rate of independence that is important in Germany.’
Toennes concedes there is a negative side, too: a lack of money. While the police pay the university for work, it’s not enough to cover all the costs. ‘It’s a problem in Germany that legal medicine is very cost intensive and universities have low budgets that are becoming more and more restricted,’ he explains. ‘And therefore, we don’t have the newest analytical equipment. A sensitive and versatile QTOF, or something like that, this is something most labs dream of.’
In Sweden and Finland the system is different again, explains Braithwaite. ‘All the work is done by large government labs that are well run, well-funded and very high quality. They are also able to do research.’
In the US the setup resembles that of the UK. Forensic toxicology is performed by a wide variety of different types of labs, explains Dan Isenschmid, a forensic toxicologist at NMS Labs, a private firm based in Willow Grove. The FBI has its own forensic toxicology labs largely for federal cases, but ‘most of the forensic toxicology is done at the state level or local level’, he says. The most populated states or counties normally have an in-house post mortem toxicology or crime laboratory, while the smaller jurisdictions use private labs. ‘But there are certainly exceptions to that where large jurisdictions do send things to commercial laboratories,’ he says. ‘There is no one-size-fits-all for this.’ In addition, some US universities do perform forensic toxicology for the police, medical examiners and coroners. ‘There are laboratories – at the University of Florida, for example – where the toxicology laboratory is a not-for-profit, fee-for-service entity under the jurisdiction of the university.’
Nina Notman is a science writer based in Salisbury, UK












No comments yet