Jamie Durrani tells the story of how a wonder drug against malaria was discovered from a plant in a secret Chinese military project
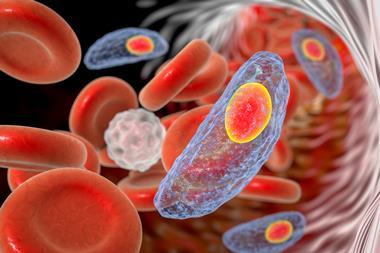
During the Vietnam war, soldiers on both sides were sent into mosquito-infested rainforest without proper protection against the disease the insects carried. By the late 1960s, the plasmodium falciparum parasites carried by mosquitos had begun developing resistance to chloroquine, a key anti-malarial that had been used extensively over the previous two decades. The result was tens of thousands of troops falling ill, and at times more soldiers were felled by malaria than actual combat.
While the US invested millions establishing a state-of-the-art malaria research unit, the North Vietnamese leader Ho Chi Minh turned to his allies in China for help. His plea triggered an extraordinary project that led to the discovery (or re-discovery) of the world’s most effective malaria treatment. Remarkably, the project took place in the throes of China’s cultural revolution, when many scientists and other intellectuals faced persecution, and much academic research had ground to a halt across the country.
Top secret
Having been informed of Ho’s call for assistance, Chinese leader Mao Zedong ordered a nationwide search for new malaria treatments. The top-secret project would be led by the military and would involve hundreds of researchers from institutions across China.
On 23 May 1967, representatives of China’s national science commission and the military assembled at a Beijing restaurant to start the operation, which was given the name Project 523 in reference to the project’s launch date. The main aim was to find fast-acting drugs that could kill drug-resistant malaria parasites with minimal side effects.
Project 523 would last for 13 years and lead to the identification of numerous compounds with antimalarial activity, as well as related products like insecticides and spray devices. The most important of these was artemisinin – a drug that is today recommended by the World Health Organisation as the first-line treatment for malaria worldwide.

Following Project 523’s launch, up to 60 military and civilian teams from across China began a nationwide search for possible malaria treatments. One branch of the project saw researchers travel to districts where malaria was endemic to gather information from local people on folklore and traditional remedies. Another branch followed a more modern approach, whereby pharmaceutical manufacturers began designing new chemical compounds and screening them for anti-malarial activity.
But by 1969, and despite testing almost 20,000 different molecules in its first two years, Project 523 had failed to produce the wonder-drug it was tasked with finding.
‘Nothing seemed to be promising. And the central leadership, the premier and vice-presidents were all asking “How are you guys doing?”‘ explains Xin-zhuan Su, who heads the malaria genomics section at the National Institute of Allergy and Infectious Diseases (NIAID) in Maryland, US. ‘So they feel pressure – real pressure – and so they start looking for additional help. And that’s how Tu got into it.’
In 1969, three Project 523 leaders visited the Institute of Chinese Materia Medica (ICMM) in Beijing, seeking help with the branch of the project that was searching through Chinese traditional medicine for potential malaria treatments. Here they approached Tu Youyou, a researcher with a unique combination of expertise in both modern scientific methods and traditional Chinese remedies. Tu was asked to lead research at the ICMM to contribute to Project 523 – work that would eventually see her rewarded with the 2015 Nobel prize in medicine for her role in artemisinin’s discovery.
Tu’s team prepared hundreds of extracts from 200 different herbs
Tu has written about the overwhelming responsibility and feeling huge pressure due to the national significance of the project, as well as the speed with which results were sought. Her involvement would also require her to spend years separated from her young children while she dedicated herself to the project. All this at a time when Tu’s own husband was interned in a re-education camp for intellectuals as part of the Cultural Revolution.
Tu’s team scoured Chinese folklore for any apparent remedies for ailments with symptoms resembling those of malaria and also interviewed practitioners of traditional medicine. Within three months the team had compiled a list of more than 2000 herbal treatments, which they shared with other research groups involved in the project. Of the 2000 remedies, 640 were considered possible hits. Based on these recipes, Tu’s team prepared hundreds of extracts from 200 different herbs.
But two years of testing herbal extracts on rodent malaria models produced little in the way of promising results, and so Tu returned to the traditional Chinese medical literature. One class of herb, commonly referred to as qinghao, had shown some positive results in malaria screens but the results had been inconsistent and not easily reproduced. Tu has described reading and re-reading passages from the Chinese pharmacopeia that described the use of qinghao.
Extraction solution
It was in one such document – the Handbook of Prescriptions for Emergency Treatments compiled by the physician Ge Hong in the year 340 CE – that Tu found a crucial clue. Hong’s handbook described a remedy for intermittent fevers – a symptom relevant to malaria. Hong instructed the user to ‘take a handful of qinghao immersed in two sheng [0.2 litres] of water, wring out the juice and drink it all’.
While most traditional recipes called for herbs to be boiled in water, Tu noted that at no point had Ge Hong instructed users to heat the water. She wondered if the methods her team used to prepare its extracts had unwittingly destroyed an active ingredient in the plant.
Tu’s team carried out extractions at low temperature using water, ethanol and diethyl ether as solvents. The ether extract in particular was found to be highly active against plasmodium falciparum parasites in mouse models.
Anthony Butler, a retired University of St Andrews biological chemist, explains that one reason the ether extract performed so much better is due to the low water solubility of qinghao’s active ingredient. It’s likely that the scientific approach taken by Tu’s team in their first experiments with qinghao actually filtered out the artemisinin, which explains the inconsistent results they had seen in malaria screens.
‘The [traditional] procedure is to soak the plant in a bucket of water and take the water and use that as a source of [artemisinin] – now, if you carefully filter it, you won’t get any result,’ says Butler. ‘How is it then that [practitioners of traditional Chinese medicine] had been able to harness its therapeutic value when they hadn’t got any organic solvent? Well, if you don’t filter it, you get bits of the plant containing artemisinin which get into the body, and it’s the body that converts it into a water-soluble version that circulates around the body.’
Most pharmaceutical workshops were shut down during the cultural revolution
While the ether extract had proven successful at killing malaria parasites, initial tests on mice also produced some unwanted toxic side effects. The team then treated their samples with an alkaline solution, to remove acidic impurities from the ether extract. Further testing of the neutralised ether extracts showed 100% efficacy in mice and monkeys infected with malaria parasites, with greatly reduced toxicity. Tu described this as the ‘critical step in the discovery of artemisinin’.
Tu reported the results to a large meeting of Project 523 participants from across China’s research institutes on 8 March 1972. The results sparked a renewed nationwide effort to harness qinghao’s antimalarial properties.
From this point, many more teams across Project 523 focused their efforts on qinghao. Tu’s team started to prepare large quantities of the extract for use in clinical trials. It was tough work and, given the lack of funding for research in China at the time, Tu’s lab had only the most basic of equipment. Members of the team, including Tu herself, have spoken about the how the poor ventilation meant that many of those working on the project started to show signs of illness brought on by the solvent fumes in the lab.
‘Most pharmaceutical workshops were shut down during the great cultural revolution,’ Tu explained in a short autobiography written for the Nobel Foundation. ‘Without manufacturing support, we had to extract herbs ourselves using household vats etc. The team worked very long hours every day including the weekends.’
While this was going on, further testing of qinghao on animal models had shown mixed results in terms of toxicity. By the midsummer in 1972, Tu offered to test the extracts on herself – reasoning that if debate over qinghao’s safety continued for much longer the malaria epidemic season would end, and full field trials would be delayed until the following year. In July 1972 Tu and two other members of her team tested the extracts under close supervision in a hospital. No side effects were seen over the following week, and so another five team members volunteered to take larger doses.
These tests cleared the way for field trials. Tu travelled to China’s most southerly province, Hainan, to oversee a trial in which 21 malaria patients were treated with the qinghao extract. Another nine patients were treated at a hospital in Beijing. All of the patients were cured of their malaria symptoms, and no parasites were detected following the treatment.
A structural problem
It’s important to note that these first trials made use of qinghao extract, rather than a single purified compound. At the same time that the trials were happening, efforts began towards fully determining the structure of the mysterious active ingredient.
Given artemisinin’s unusual structure, and the limited equipment available to the Chinese researchers in the early 1970s, this was no simple task. In November 1972, a member of Tu’s team, Zhong Yurong, managed to obtain crystalline samples of different materials present in the qinghao extract, determining that a sample dubbed ‘qinghaosu II’ was the active ingredient.
A series of analytical experiments completed by April 1973 established the C15H22O5 formula, but a full structure would take another four years. One issue was the difficulty in obtaining high quality crystalline samples.
‘One of the reasons is the artemisinin is only [in] the young leaf of the plants, and they didn’t realise that,’ says Su. ‘The other issue is different plants growing in different regions have very different contents. In other words, if you get the plant from the central Sichuan province, it’s 10 times higher concentration than if you get it from Beijing.’
Su notes that researchers led by Luo Zeyuan at the Yunnan Institute of Pharmacology and Wei Zhangxing at the Shandong Institute of Chinese Traditional Medicine were able to drastically improve the methods for obtaining artemisinin crystals. A major breakthrough was the discovery that of the six species traditionally referred to as qinghao, only the sweet wormwood plant (Artemisia annua, known locally as huanghua hao) contained sufficient quantities of artemisinin.
‘[The Yunnan institute] was able to get the plant with a high concentration on the leaf. And they also modified the methods – when producing large amounts you cannot keep using ether, because it’s toxic and expensive. So eventually they used gasoline, regular gas, and now they could produce a ton of crystals very quickly. So that is a very big contribution.’
The first papers on artemisinin – the whole story – were published in Chinese journals
The crystals were used in x-ray studies at the Institute of Biophysics at the Chinese Academy of Sciences in Beijing that finally revealed artemisinin’s remarkable structure – a sesquiterpene lactone containing a highly unusual peroxide bridge.
‘Seven-membered rings are rare amongst natural products. So you’ve got a rather unusual structure for a start. But above and beyond that, the seven membered ring has an oxygen–oxygen bridge across it,’ says Butler. ‘Now oxygen–oxygen bonds are very weak and normally fall apart. But the one in artemisinin seems to be quite stable, you can heat it to 100°C, and it won’t decompose. And this is very strange and very unexpected.’
Due to the clandestine nature of Project 523, details of artemisinin and its antimalarial activity were closely guarded by the project’s leadership. The single-page paper describing artemisinin’s crystal structure published anonymously in 1977 in the Chinese language journal Kexue Tongbao marked the first time that any information was released publicly. A series of follow-up papers were published in 1979, providing the first information on artemisinin’s efficacy against malaria parasites.
‘The first papers on [artemisinin] – the whole story, the crystal structure, everything about it was published in Chinese journals, and there were no authors. Institutions, but no authors; it was very strange,’ says Louis Miller, the head of NIAID’s malaria cell biology section, who alongside Su has carried out meticulous research into the story of artemisinin’s discovery.
While artemisinin’s exact mode of action still hasn’t been fully elucidated, it is clear that the peroxide bridge is key to its antimalarial properties. In the presence of iron, the oxygen bridge decomposes to produce destructive radical species. ‘This radical can attack nearby structures such as proteins, and heme itself,’ says Caroline Ng, a microbiologist at the University of Nebraska in the US. ‘And so we think that this non-specific alkylation of nearby proteins causes a lot of protein damage, and thus the parasite can’t survive.’
‘Three different groups, when they looked at what was being alkylated in the parasite, [found] there was very little overlap in the proteins that they identified,’ she adds. ‘So this is why we think there is nonspecific alkylation.’
In the years that followed the initial discovery of artemisinin’s antimalarial activity, a much wider Project 523 effort would conduct larger trials, ultimately leading to approval of artemisinin from China’s Ministry of Health in 1986. This would be followed by approvals for other drugs derived from artemisinin, including a more potent derivative called dihydroartemisinin, which Tu discovered in 1973.
Modern treatment
Over the following decade extensive work across China confirmed the safety and efficacy of artemisinin and its derivatives, but it took much longer for the drug to gain approvals for use around the world. In fact, it wasn’t until 2006 that the WHO began recommending artemisinin-based therapies as the first-line malaria treatment worldwide.

Some researchers have argued that the reason it took so long for western scientists to approve the qinghao derived drugs was due to prejudice – disbelief that Chinese scholars cut off from the rest of the world and with outdated equipment could really have developed such a ‘wonder-drug’. However, it is important to note that even the leaders of Project 523 acknowledged that, as China opened up to the world, the country’s pharmaceutical manufacturers needed to significantly upgrade their facilities to comply with international standards for good manufacturing practice.
Another factor that could explain why researchers outside of China were slow to pick up on artemisinin’s potential is the fact that the drug is eliminated from the body very quickly. This means that a single dose of artemisinin won’t kill all of the malaria parasites in a patient and the malaria symptoms will soon return.
‘If you give artemisinin alone to a patient, you’re going to see the parasites go down quickly – it starts to kill parasite in about 40 minutes,’ says Su. ‘But it doesn’t clear totally, so the parasites will come back. So initially, if you don’t do a so-called combination therapy, you are going to see this drug is a failure.’
Today, artemisinin combination therapies (ACTs) are the recommended treatments for malaria, with Novartis – working with Chinese partners – having supplied more than 1 billion ACT courses without profit over the last two decades. As the name suggests, these therapies combine artemisinin-based drugs with other anti-malarials that help to remove more of the parasites, until a full treatment programme over a few days leads to complete clearance.
The only drugs that have persisted in efficacy against malaria are both plant products
But the fact that artemisinin is so effective at treating the symptoms of malaria is beginning to cause concern among medical researchers. ‘At the moment, artemisinin is given as three doses over three days and that presumably leads to non-compliance, especially on the second and third day – because artemisinin is so good and it reduces parasite biomass so quickly, that you do feel better after the first day,’ explains Ng. ‘And then because drugs are expensive, workers will tend to keep the drugs for the next time they get sick. And unfortunately, this leads to sub-dosing of the parasite.’
This non-completion of treatment programmes, as well as the inappropriate use of artemisinin as a monotherapy, has led to fears that malaria parasites could develop resistance to the drug. Many researchers have observed an increase in the time taken for parasites to be cleared by artemisinin therapies
Su notes that, unlike other anti-malarials to which parasites have developed much stronger resistance, a full course of artemisinin treatment should still cure the illness, even if the drug needs to be taken in slightly higher doses, or over a longer period. ‘Artemisinin oxidises about 100 proteins, so [for the parasite] to develop resistance is not easy,’ he says. ‘So we don’t have the typical definition of resistance, there’s just one particular definition – delayed clearance – for artemisinin.’
‘To date the only drugs that have persisted in efficacy are quinine and artemisinin, and both are plant products,’ adds Miller. ‘It’s interesting, because the synthetic things we come up with, the parasites are pretty good at getting around them.’ He notes that this vulnerability to resistance, as well as high cost, means that some synthetic anti-malarials are solely reserved for western travellers and not used for local populations.
‘The point is that if it’s expensive and the developing world can’t use it, then it stays effective. And that’s what makes artemisinin so wonderful – that it does work, and resistance is not a problem, and it continues to work, whereas all the synthetics seem to be a problem,’ says Miller. ‘Now, whether that will continue to be, I don’t know.’
Jamie Durrani is a science correspondent for Chemistry World













No comments yet