Amplifying or silencing genes may be preferable to permanently changing genetic code
Genetic engineering is difficult. And the consequences can be unpredictable. It’s therefore unsurprising that commercial efforts have often met with significant public and political resistance.

In food crops, methods that introduce genes for desirable traits from other species have seen more opposition than techniques that work more like accelerated versions of conventional plant breeding (including using Crispr gene editing). A new generation of edited foods is now emerging, as regulations begin to distinguish the two.
But in humans – and to some extent animals – even Crispr-style editing has significant risks, because the changes are permanent, and off-target edits can have serious consequences. Companies trying to develop Crispr-based therapies have discovered that delivering editing machinery accurately in a living organism is harder than they expected. Partly that’s down to the size of the Crispr-Cas complexes and the physical challenge of delivering them, but also the realisation that the technique is a little more promiscuous than anticipated.
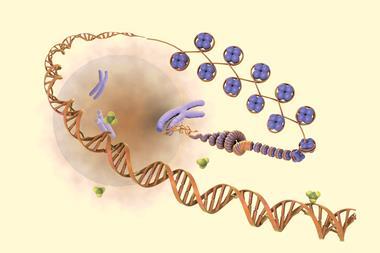
That is where epigenetic therapies – which amplify or silence genes without altering genetic code – could come into their own. The protein machinery required can, in some cases, be much smaller than for Crispr editing, making it easier to package into a variety of drug delivery vectors. Rather than making permanent cuts to DNA, epigenetics harnesses the DNA-tagging process that controls how strongly genes are expressed. And because it takes quite a lot of tagging to significantly influence a gene’s expression, the consequences of an occasional off-target tag are minimal.
In theory, epigenetic therapies could employ different tags to either increase or decrease expression of genes, but all the therapies currently approaching or entering clinical trials have opted to completely silence over-active genes using methylation. Focusing on this approach before attempting tuned amplification of under-expressed genes is understandable. Turning a gene off is much easier than turning it on, and it’s not a huge issue if you overdo the silencing a little. On the other hand, over-activating a gene could easily lead to problematic side effects. Convincing regulators, doctors and patients that a very different type of therapy is safe and effective is (rightly) a high bar to pass, so starting easy is sensible.
Which brings us to another looming challenge. Most of the companies developing epigenetic therapies are based in the US. But with the US Food and Drug Administration in turmoil under its new leadership, it’s unclear how much of its stretched resources it will be able to dedicate to working out the regulatory pathways for a whole new class of therapies. While the US has previously prided itself on its receptiveness to innovative new medicines, it’s possible these companies may end up facing frustrating delays, or even looking elsewhere for their initial approvals.
















No comments yet